Gastroschisis In Newborns
Gastroschisis is one of the most frequent congenital malformations. However, in turn, it is unknown to most of the population. This malformation occurs when the muscles of the baby’s abdominal wall are not formed correctly in early pregnancy.
In this way, a hole is created through which the intestines and other organs of the child exit. Usually it is towards the right side of the navel. Because the intestines are exposed to amniotic fluid, they can become irritated, for this reason they can shorten, swell, or twist.
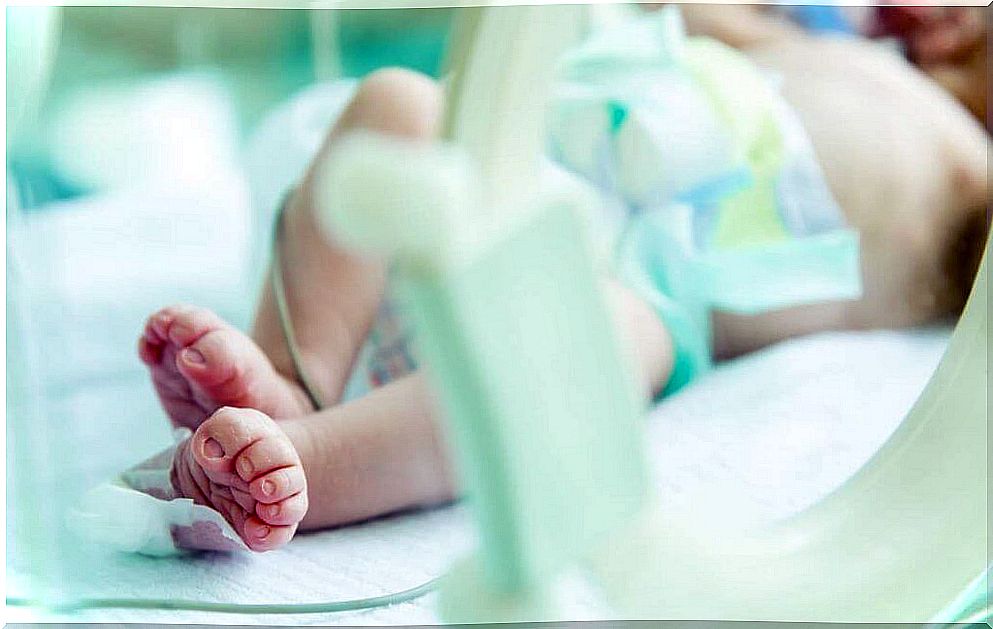
Right after birth, the newborn will require surgery to place the organs inside, as well as to repair the abdominal wall. Despite surgery, babies with gastroschisis may have problems with feeding, digestion, and absorption of nutrients.
Causes and risk factors of gastroschisis
Some of the cases of gastroschisis are due to changes in the genes, as this study published in the American Journal of Medical Genetics Part A points out , although on other occasions it may have its origin in the combination of genetic factors and factors related to the mother during pregnancy. As for the factors that increase the risk of having a baby with gastroschisis are the following:
- Being a mother at an early age : Teen mothers are more likely to have a baby with gastroschisis than older mothers.
- Tobacco and alcohol consumption : Women who smoke and consume alcohol are at higher risk of having babies with gastroschisis.
All of this is evidenced in this information from the Centers for Disease Control and Prevention (CDC).
Diagnosis and treatment
Diagnosis can be prior to birth or as soon as the baby is born. During pregnancy, malformations detection tests are carried out, therefore, with specific tests it can be detected. In addition, it is seen on an ultrasound.
In terms of treatment, gastroschisis is a life-threatening condition. You need treatment as soon as possible after birth so that the baby’s organs can develop and are protected within the abdomen.
In the event that the defect is small, it will be repaired in a single intervention. However , if it is a large defect in which many organs come out, the repair can be done in stages, as this research paper published in the journal Surgical technology international points out . After the surgery is done, the baby goes to the neonatal intensive care unit.
Risks of surgery
The risks of anesthesia and general surgery are
- Allergic reactions to medications.
- Respiratory problems.
- Infection and bleeding
Regarding the risks involved in gastroschisis repair are the following:
- Organ injury.
- Hernia of the abdominal wall.
- Temporary paralysis of the small intestine.
- Inflammation of the tissue that lines the abdominal wall.
- Respiratory problems : can appear if the baby’s abdominal space is smaller than normal. The newborn may need a breathing tube and aspirator for a few days or weeks after surgery.
Complementary treatments

In addition to surgery, babies with gastroschisis often need other treatments as well, such as:
- Oxygen.
- Analgesics.
- Antibiotics to prevent infection.
- Fluids and nutrients through a vein.
- Nutrition by nasogastric tube placed in the nose to empty the stomach and keep it that way.
Feeding begins by nasogastric tube as soon as the baby’s bowel function resumes after surgery. However, oral feeding will be done very slowly, gradually. Medical discharge is usually given within a period between 15 and 25 days after admission.
Prevention of gastroschisis
Prevention consists of having adequate prenatal care with healthy habits and attending the necessary consultations to prevent complications. Once the diagnosis is made, specialized care and adequate follow-up are needed.
In these cases, ultrasound plays a prominent role. Weekly ultrasound control is recommended after 30 weeks of gestation.
Newborns with gastroschisis are generally underweight, and 10-20% have intestinal malformations. However, the degree of intestinal suffering will determine, to a large extent, the prognosis of these little ones.
However, in recent years, survival has improved dramatically. This is due to early detection and the application of prenatal follow-up protocols, as well as appropriate intensive care.