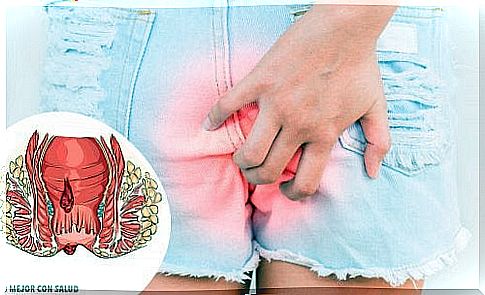
Treatment Of Anal Fissure
An anal fissure is the reduced tearing that takes place in the anal mucosa, which is a thin and moist tissue, so tears are a common problem. It is an alteration that can be suffered at any age, although it often appears in babies and young children.
We can place this problem in the final section of the large intestine, in the anus. This hole is the communication of the final part of the intestine with the outside. The condition usually takes place on the back or outside of the anus.
Types of anal fissure

According to various variable factors within this disorder, we can distinguish, for example, between:
- Acute or chronic anal fissure. To do this, the duration, location and if the anal fissure is recurrent (it appears frequently) are reviewed. If the alteration lasts for less than six weeks and has not developed in recent years, it is acute. On the other hand, if the fissure appears frequently and with a longer duration, it is classified as chronic.
- Primary or secondary anal fissure. In the first case, the cause is mechanical (physical) or unknown. In the second case, the problem presents an underlying disease that causes the anal fissure.
What are the symptoms of anal fissure?
Frequently, the patient presents a series of symptoms and signs that can be related to this disorder. Among the most common we can highlight:
- Severe pain during and after bowel movements. In some clinical cases, the discomfort may have lasted for hours after defecation.
- Presence of blood in the area near the anus due to slight exertional bleeding.
- Itching or irritation around this body area.
- Formation of small cracks in the skin around the anus. Small lumps may also develop.
What are the causes of anal fissure?
Currently, specialists have been able to identify a series of triggers or risk factors that cause anal fissure. We mention the most common:
- Passing of large or hard stools.
- Constipation. The effort that the patient makes to try to evacuate translates into an overload of the sphincters. The sphincters are the muscles responsible for increasing and decreasing the diameter of the anus.
- Chronic diarrhea.
- Recent delivery.
- Diseases that directly affect the anorectal region (such as Crohn’s disease).
- Other pathologies such as tuberculosis, HIV, etc.
What is the treatment of anal fissure?
Today, new techniques have been developed to calm the patient’s discomfort. Other guidelines to do at home related to a number of healthy habits are also recommended.
However, in more severe clinical cases, the subject may need to undergo surgery. Thus, surgical intervention is applied to solve complications. In this way, we can distinguish between:
Guidelines for adapting the patient’s lifestyle
As a general rule, anal fissures usually heal on their own in a few days or weeks. For example, specialists recommend a diet rich in fiber and plenty of fluids.
Thus, the stool becomes softer and discomfort during bowel movements is reduced . Taking baths with hot water for a few minutes each day is also recommended. The resulting relaxation helps unload the sphincters, speeding up healing.
Treatments that do not include surgery
Among the most used compounds we find, for example:
- Local anesthetic creams. They work by relieving pain in the affected area.
- Injection of botox (botulinum toxin type A) to paralyze and relax the sphincter of the anus.
- Nitroglycerin for external use. It is a compound that is capable of increasing blood flow to the fissure. Causes relaxation of the sphincter and increases the speed of tissue healing.
Surgical procedures
Experts perform a lateral internal sphincterotomy, or ELI. In it, a small portion of the problem muscle (anal sphincter) is removed. In this way, the discomfort progressively decreases in intensity and regeneration is promoted.
Conclution
Anal fissure is a very annoying ailment that always requires the observation of a medical professional. It generally heals without complications, but may occasionally require specialized treatment.
Remember that in case you have concerns, it is best to consult with your doctor. Avoid resorting to self-medication and natural remedies, as they could be counterproductive.